比较咪达唑仑、丙泊酚、右美托咪定镇静对急性心肌梗死危重患者预后的影响
文章插图
贵州医科大学麻醉与心脏电生理课题组
翻译:任文鑫 编辑:陈锐 审校:曹莹
HOLIDAY
背景
关于急性心肌梗死(AMI)危重患者镇静治疗的研究较少。本研究旨在比较咪达唑仑、丙泊酚和右美托咪定对AMI危重患者预后的影响。
HOLIDAY
方法
我们从重症监护III医疗信息集市(MIMIC III)数据库收集临床数据。427例使用镇静剂的AMI患者的数据来自冠心病重症监护病房(CCU)。从冠心病重症监护病房(CCU)采集了427名使用镇静剂的AMI患者的数据。
HOLIDAY结果
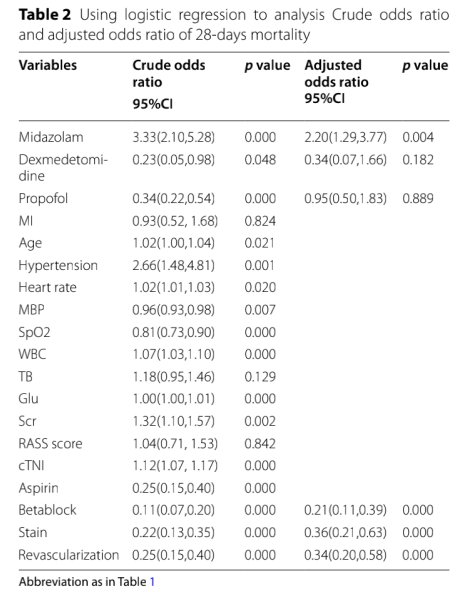
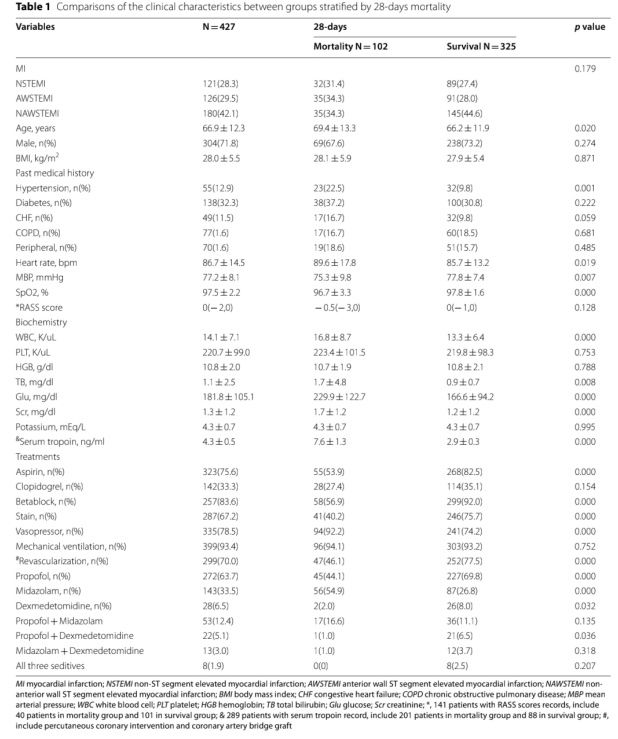
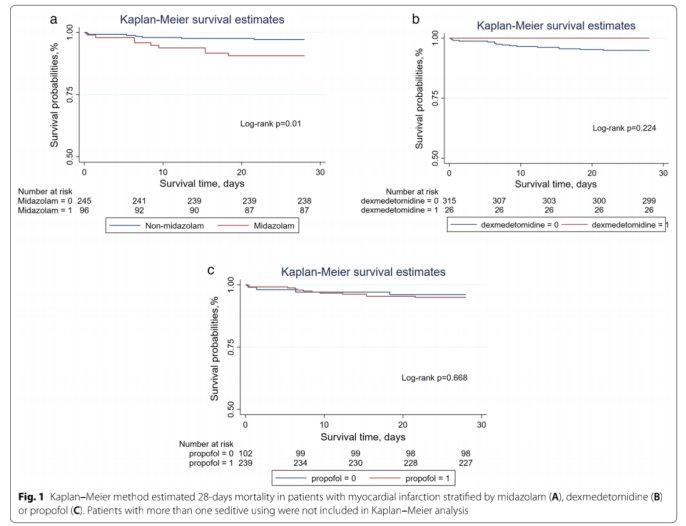
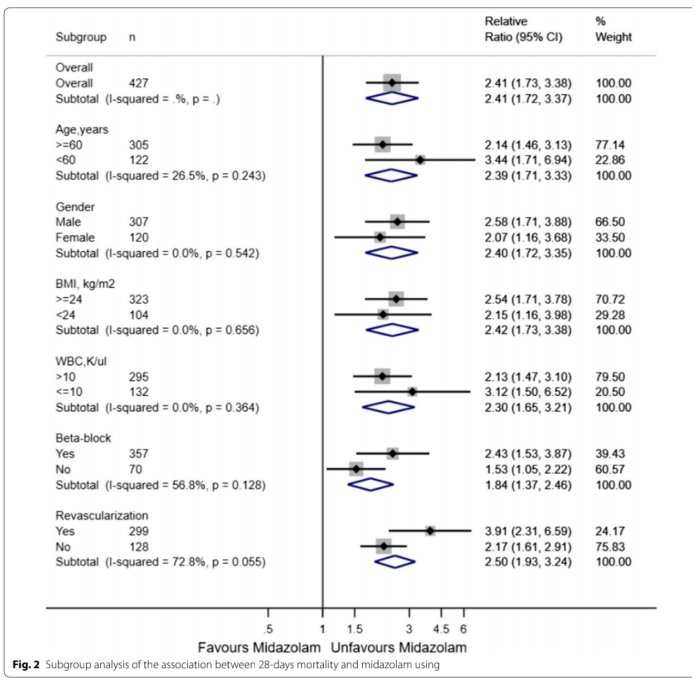
使用咪达唑仑患者有143例,使用丙泊酚患者有272例,使用右美托咪定患者有28例。总体患者28天死亡率为23.9%。通过逻辑回归分析结果表明,与使用丙泊酚或右美托咪定的患者相比,仅使用咪达唑仑的患者与增加28天死亡率显著相关。在年龄、性别、体重指数(BMI)、白细胞(WBC)、β受体阻滞剂和血运重建的亚组分析中,使用咪达唑仑与增加28天死亡率之间的相关性仍然显著。通过倾向评分匹配,140名使用咪达唑仑的患者和192名使用非咪达唑仑的患者成功匹配,使用咪达唑仑的患者CCU死亡率、住院死亡率和28天死亡率较高,机械通气时间和CCU持续时间较长。E值分析表明对未测量的混杂因素具有稳健性。
文章插图
文章插图
文章插图
文章插图
HOLIDAY结论
AMI危重患者首选丙泊酚或右美托咪定进行镇静治疗。
HOLIDAY 原始文献来源
Xiaowei Jiang,Min Yan.Comparing the impact on the prognosis
of acute myocardial infarction critical patients of using midazolam, propofol, and dexmedetomidine for sedation.Jiang and Yan BMC Cardiovascular Disorders (2021) 21:584.
Comparing the impact on the prognosis of acute myocardial infarction critical patients of using midazolam, propofol, and dexmedetomidine for sedation
Abstract
Background: There are less studies focusing on the sedative therapy of acute myocardial infarction (AMI) critical patients. This study aim to compare the impact on the prognosis of AMI critical patients of using midazolam, propofol and dexmedetomidine.
Methods: We collected clinical data from the Medical Information Mart for Intensive Care III (MIMIC III) database. Data on 427 AMI patients with sedatives using were recruited from in Coronary Heart Disease Intensive Care unit (CCU).
Results: There were 143 patients in midazolam using, 272 in propofol using and 28 in dexmedetomidine using. The rate of 28-days mortality was 23.9% in overall patients. Through logistic regression analysis, only midazolam using was signifcant association with increased 28-days mortality when compared with propofol or dexmedetomidine using. In the subgroup analysis of age, gender, body mass index (BMI), white blood cell (WBC), beta-block, and revascularization, the association between midazolam using and increased 28-days mortality remained signifcantly. Through propensity score matching, 140 patients using midazolam and 192 using non-midazolam were successfullymatched, the midazolam using presented with higher rate of CCU mortality, hospital mortality and 28-days mortality, longer of mechanical ventilation time and CCU duration. E-value analysis suggested robustness to unmeasured confounding.
【 急性心肌梗死|【罂粟摘要】比较咪达唑仑、丙泊酚、右美托咪定镇静对急性心肌梗死危重患者预后的影响】 Conclusion: Propofol or dexmedetomidine are preferred to be used in AMI critical patients for sedative therapy.
- 主动脉夹层|晨读丨1月27日,关注健康每一天
- 社交边界感有多重要
- 评分|《神秘海域:盗贼合集》M站媒体评分解禁 均分88分
- 两个人一直腻在一起是怎样的体验?
- 宇宙的裂缝
- 心电图|【科普】心电图上的窦性心律不齐是心脏病吗?
- 血脂异常|《脑心同治 医者语录》 ——陈伯钧:预防心脑血管病要从青年开始
- 知识|冬季养生保健知识
- 水满则溢,月满则亏,为人处事把握“这个字”,方能悠然自得
- 夜读 | 过年你回家吗?
